On World Diabetes Day 2025, the global theme “Diabetes across life stages” highlights the need for integrated care and support for people living with diabetes at every age. Imagine a future where every third person you meet is living with diabetes – a silent but relentless epidemic quietly engulfing India’s societal fabric. In 2025, estimates reveal that nearly 90 million adults are battling this chronic disease, with millions more unaware that they are affected. Astonishingly, India’s diabetes burden has skyrocketed so rapidly that it now surpasses many infectious diseases in its social and economic toll. What if I told you that this crisis isn’t just about health – it’s about a fundamental restructuring of life itself? As urban lifestyles change, childhood habits erode, and healthcare systems strain, the battle across all ages intensifies, demanding urgent, systemic action.
Certainly, the numbers speak a story of urgency. Increasingly, it is a story of missed opportunities for early diagnosis and prevention, of social stigma, and of health inequities widening daily. Moreover, the rise from 69 million cases in 2015 to nearly 90 million in 2025 signals a crisis that threatens to overwhelm families, workplaces, and governments across India. Yet, amid this alarming surge, there is hope – if we understand the scope, learn from history, and adopt innovative strategies to combat diabetes. On this World Diabetes Day, the fight against diabetes in India is not just medical; it is a societal revolution begging for collective action and conscious change.
Diabetes in India: A Historic and Statistical Overview
Diabetes prevalence in India has experienced a worrying rise over the last three decades. It was relatively rare in the early 20th century but has morphed into an epidemic over the last 50 years, fuelled by rapid urbanization, lifestyle changes, and genetic predisposition. Current estimates rank India as the second-highest diabetes-burdened country globally, with roughly 89.8 million adults living with the disease in 2025. This marks a steep increase from approximately 69 million cases in 2015, according to the International Diabetes Federation (IDF).
For context, India’s share of global diabetes cases increased dramatically post-1990 as economic liberalization accelerated lifestyle shifts – sedentary work, processed foods, and reduced physical activity became the new norm. Dr. Pranav Ghody, a leading diabetologist, encapsulates this progression: “India has earned the title of the diabetes capital of the world.” This is not mere hyperbole; it reflects a public health reality that is straining healthcare resources and families alike. Furthermore, the ripple effects extend beyond individual illness. The International Diabetes Federation projects that India’s total healthcare expenditure on diabetes will surpass ₹1.26 lakh crore in 2025, making diabetes not just a medical concern but a significant economic challenge.
Diabetes Prevalence in India (2015-2025)
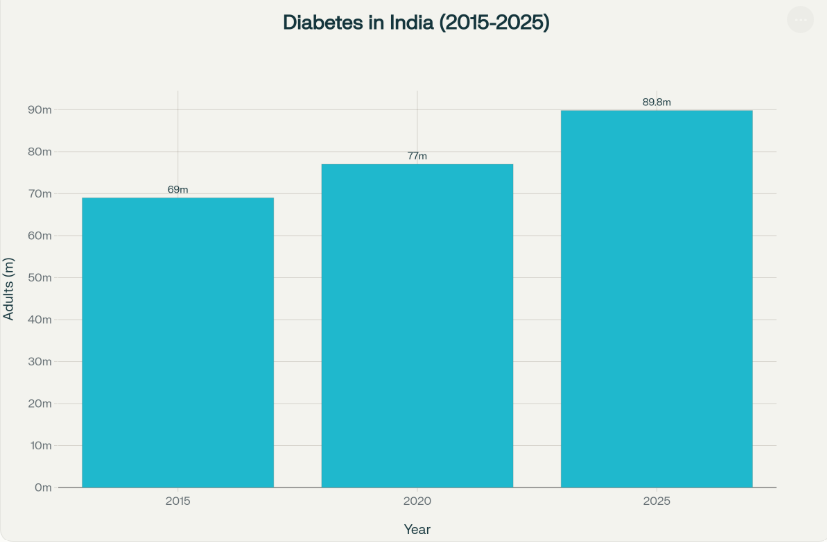
Source: IDF Diabetes Atlas, WHO, National Health Surveys
World Diabetes Day 2025 Theme: Across Life Stages
First and foremost, the 2025 theme emphasizes diabetes management at all life stages. Children, young adults, and the elderly equally face risks requiring targeted interventions. Schools need greater focus on early detection and lifestyle education nationwide. Simultaneously, seniors must access consistent care to prevent complications effectively. Dr. Sanjay Agrawal emphasizes, “Diabetes prevention must become a national priority” in India. This holistic approach broadens support across healthcare systems and communities alike.
Besides, inclusive care combats stigma that often isolates affected individuals across age groups. Consequently, efforts to connect families, workplaces, and healthcare providers gain importance urgently. Health policies should prioritize integrated screening, treatment, and continuous education nationally. Moreover, sustaining lifestyle changes requires community solidarity fostering healthier habits collectively. Will India rise to empower citizens in this fight across generations soon?
Urban Dietary Transitions and Diabetes
Meanwhile, India’s transition toward processed, sugary foods accelerates diabetes prevalence sharply. Urban diets often replace traditional meals with high-calorie, low-nutrient convenience foods. Ironically, despite better awareness, unhealthy eating remains common and culturally promoted regularly. Traditional, nutrient-rich diets are often replaced by calorie-dense, ultra-processed foods high in sugar, fried snacks, sugary drinks, saturated fats, and refined carbohydrates. Such urban dietary transitions contribute directly to rising rates of insulin resistance and Type 2 diabetes. Health experts advocate dietary shifts toward whole grains, fruits, vegetables, and legumes instead. This nutritional awareness represents a critical lever for diabetes prevention immediately.
Furthermore, sedentary lifestyles in urban areas amplify risk significantly alongside poor diet choices. Increased screen time, mechanized transport, and desk jobs limit daily physical activity greatly. Consequently, obesity and metabolic disorders rise concomitantly, deepening diabetes vulnerability further. Ironically, despite increased awareness campaigns, unhealthy eating habits persist among all socio-economic classes, partly driven by marketing influences and busy lifestyles. Public policies imposing sugar taxes, promoting labelling, and banning junk food ads could prompt healthier options. However, consumer awareness and willpower remain vital determinants of dietary change. Can urban India revert to nourishing traditions before diabetes overwhelms?
Diabetes Awareness Campaigns and Early Detection
Notably, awareness campaigns have significantly increased diabetes knowledge across Indian populations recently. Research Society for the Study of Diabetes in India (RSSDI)’s Defeat Diabetes Campaign and governmental “75 by 25” initiative symbolize these massive outreach efforts. Millions now attend screening camps and educational workshops annually, raising early diagnosis rates. Nevertheless, awareness gaps persist strongly in rural and socioeconomically disadvantaged communities. Dr. Rajesh Kesari highlights, “Diabetes prevention is our collective responsibility,” inspiring collaborative action.
Moreover, pervasive stigma often delays care-seeking and complicates management for affected individuals. Therefore, counseling and peer support networks emerge as essential complements to medical treatment. Improved patient education on medication adherence and lifestyle modifications remains critical. Digital platforms extend outreach powerfully but require equitable access expansion further. Early detection through sustained campaigns thus offers the best hope for reducing complications nationally.
Glycemic Status of Indian Adults (2025)
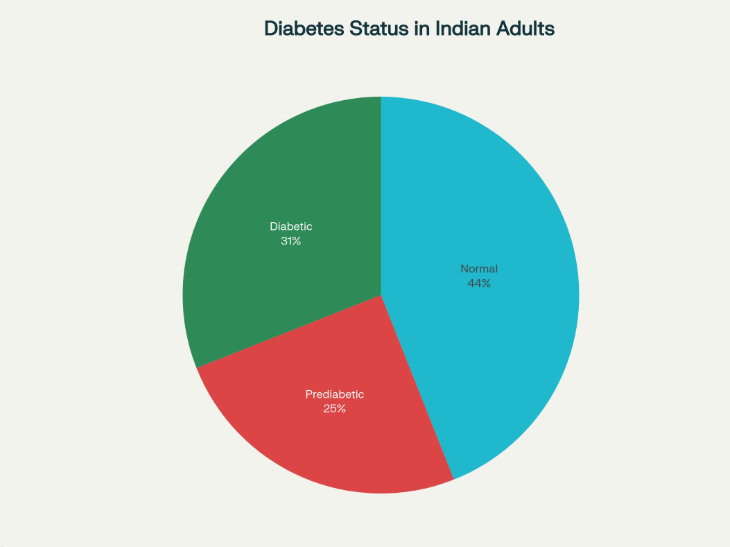
Source: PharmEasy, WHO, IDF Diabetes Reports
Economic and Workplace Impact of Diabetes
Diabetes has become a significant economic burden in India, with total healthcare expenditures related to the disease projected to reach approximately ₹1.26 lakh crore by 2025, a massive increase from ₹10,000 crore in 2003. This rise reflects not only treatment costs but also indirect expenses like lost income and productivity. Many families bear catastrophic health expenses exceeding 10% of their annual income, especially those managing complications. From my observations, this financial impact often traps families in cycles of poverty and limits access to adequate care. Therefore, addressing the economic consequences is as vital as improving medical treatment itself.
Furthermore, diabetes profoundly affects the workplace, leading to reduced productivity and increased absenteeism. Companies bear hidden costs due to employees struggling with unmanaged diabetes, affecting overall efficiency. Studies show that loss of wages and workdays is a predominant indirect cost linked to diabetes management. Fortunately, initiatives focusing on early diagnosis and employee wellness can mitigate these effects. As Dr. Sahoo observes, “Early diagnosis empowers people to manage their health proactively.” Expanding workplace health programs nationwide could significantly reduce both personal and economic burdens, promoting healthier, more productive workforces across India.
Youth and Diabetes: Alarming Trends Among Gen Z and Millennials
Youth diabetes is an emerging crisis in India, especially among Gen Z and millennials. Recent studies indicate a sharp rise in prediabetes prevalence within these age groups, with sedentary lifestyles and unhealthy diets as major contributors. Increasing consumption of processed foods, sugary beverages, and erratic eating patterns exacerbate insulin resistance significantly. Additionally, academic and work-related stress, combined with widespread screen addiction, reduces physical activity further. From my personal experience, I see many young people neglecting their health until symptoms become severe. This trend poses a ticking time bomb, threatening the nation’s future workforce and healthcare system extensively.
However, early screening and lifestyle interventions can drastically alter this trajectory if implemented promptly. Healthcare experts recommend regular glucose testing starting before age 30, especially for high-risk individuals with family history or obesity. Digital tools like health apps and wearables offer promising ways to engage youth in monitoring their well-being proactively. However, technology alone is insufficient without motivation and education addressing behavioral change. I believe integrating diabetes awareness into school curricula and workplace wellness programs can significantly reduce this rising burden. Therefore, collective efforts targeting youth must become a national priority, emphasizing prevention rather than just treatment.
Mental Health and Diabetes: A Crucial Nexus
The connection between mental health and diabetes is profound and often overlooked. Studies show that nearly 30% of people with diabetes experience depression or anxiety, which can hinder disease management significantly. Emotional stress influences blood sugar levels directly, creating a vicious cycle that worsens both conditions. From my experience of interacting with patients, I’ve seen how mental health struggles lead to neglect of medication, diet, and exercise. Therefore, integrating psychological support into diabetes care is not optional but essential. Addressing mental health improves adherence, reduces complications, and enhances overall quality of life measurably.
Furthermore, stigma and isolation around diabetes compounds psychological distress, especially in India’s social context. Support groups, counseling, and family involvement play critical roles in fostering resilience and emotional well-being. Dr. Pranav Ghody rightly stresses, “Empathy is as vital as education” in managing diabetes comprehensively. Digital mental health platforms and telecounseling services are emerging as accessible tools, especially important during pandemic and post-pandemic times. Ultimately, a holistic approach that treats both mind and body will yield the best outcomes in diabetes care nationwide.
Digital Innovations in Diabetes Management
Digital health technologies are revolutionizing diabetes care in India, enhancing accessibility and personalization significantly. Continuous glucose monitors (CGMs), mobile health apps, and telemedicine consultations are increasingly common, enabling real-time monitoring and remote support. For many patients, these tools offer newfound independence and improved adherence to treatment plans, especially in urban areas. I believe these innovations hold immense potential to reduce diabetes complications by facilitating timely intervention. However, challenges remain regarding affordability and digital literacy among rural and economically disadvantaged populations. Consequently, bridging this digital divide is essential for equitable diabetes management.
Moreover, government initiatives like the National NCD Portal have begun integrating digital tracking for millions of diabetic patients nationwide. These platforms facilitate data collection, personalized reminders, and streamlined care coordination between patients and healthcare providers. Importantly, AI-powered analytics predict risks and optimize treatment adjustments, improving outcomes. Yet, widespread implementation requires robust infrastructure alongside patient education to maximize benefits fully. In my opinion, investing in digital health infrastructure must accompany traditional healthcare improvements to tackle diabetes comprehensively across India’s diverse regions.
Modern and Affordable Diabetes Care Treatment Options in India
India offers several budget-friendly yet effective diabetes treatment options, blending conventional medicine with lifestyle modifications. Metformin remains the cornerstone drug for managing type 2 diabetes due to its safety, affordability (prices range between ₹20 to ₹50 per strip), and proven efficacy. Besides Metformin, Sulfonylureas and DPP-4 inhibitors, which are available as cost-effective generic versions, are commonly prescribed in combination therapies to optimize blood sugar control. Moreover, newer classes like SGLT2 inhibitors – such as generic Empagliflozin – are becoming more accessible, costing roughly ₹9 to ₹14 per tablet after generics entered the market recently. These advancements make modern treatments affordable for a larger population.
Naturally, treatment is not limited to drugs alone; lifestyle interventions like regular physical activity, dietary adjustments, and weight management are critical and free components of effective diabetes control. Additionally, telemedicine and digital health platforms offer accessible consultations and continuous monitoring without high costs. Programs such as government initiatives supplying essential medicines increase affordability for low-income populations. In my view, this multi-pronged approach combining generic drugs, lifestyle changes, and telehealth is transforming diabetes care in India – making it more inclusive without sacrificing quality. However, expanded insurance coverage and patient education remain vital to further improve access and adherence nationwide.
Challenges and Solutions in Rural Diabetes Care
Diabetes care in rural India faces significant challenges that hinder effective management and control. According to recent studies, nearly 37% of rural individuals with diabetes remain undiagnosed, compared to 23% in urban areas, highlighting severe disparities in awareness and diagnosis. Limited access to healthcare facilities, scarce specialist doctors, and inadequate diagnostic infrastructure exacerbate these challenges. Furthermore, financial constraints and lower health literacy contribute to poor treatment adherence and glycemic control. From my perspective, these barriers create a vicious cycle that allows complications to worsen, placing an additional burden on families and the healthcare system alike. In this context, enhancing rural healthcare infrastructure must be a priority to address this growing crisis.
Promisingly, multiple solutions are emerging to combat these difficulties in rural diabetes care. Mobile health clinics and telemedicine services improve access to screening and ongoing monitoring in remote areas. Moreover, government programs supplying essential medicines at subsidized rates help reduce financial barriers for rural patients. Community health workers trained in diabetes management play an important role in raising awareness, educating patients, and supporting treatment adherence locally. Lifestyle counseling tailored to cultural contexts further promotes effective glycemic control. In my view, combining technological innovations with grassroots healthcare workforce development provides a scalable and sustainable path forward for rural India’s diabetes epidemic. Policies focusing on these integrated strategies will be crucial to ensuring no one is left behind in the fight against diabetes
Caregivers: Pillars of Diabetes Support and Management
Caregivers play an indispensable role in managing diabetes, often serving as the backbone of support for patients. Studies reveal that 50 to 75 percent of adults with diabetes in India have active caregivers involved in their health management. These caregivers assist with daily tasks such as medication adherence, blood sugar monitoring, appointment scheduling, and dietary management. From my perspective, the presence of a dedicated caregiver can significantly improve a patient’s glycemic control and overall quality of life. However, despite their importance, many caregivers lack formal training or resources, which can limit their effectiveness. Therefore, empowering caregivers through education and support is critical for improving diabetes outcomes.
Furthermore, caregivers provide invaluable emotional and motivational support, helping patients cope with the psychological complexities of living with diabetes. They often encourage healthy habits like regular exercise and balanced nutrition, which are vital for long-term disease management. Additionally, caregivers facilitate communication between patients and healthcare providers, helping to advocate for better care. Recognizing the physical and emotional burden caregivers bear, support systems must address caregiver burnout to sustain their involvement effectively. I believe that by strengthening caregiver networks and integrating them more formally into diabetes care teams, India can vastly enhance disease management and patient well-being nationwide.
Recent News, Government Efforts and Future Directions
The Indian government has launched ambitious initiatives to tackle the diabetes epidemic effectively. Foremost among these is the “75/25” Roadmap, aiming to provide standardized care to 75 million people with diabetes and hypertension by 2025. So far, as of early 2025, over 25 million diabetics are receiving treatment under this initiative, achieving nearly 90% of the target. Additionally, nationwide screening campaigns target individuals aged 30 and above to ensure early detection and intervention. From my viewpoint, these efforts represent a critical shift toward prioritizing non-communicable diseases in India’s public health agenda. However, sustaining momentum requires continued resource allocation, healthcare worker training, and community engagement.
Moreover, future strategies increasingly emphasize technology and integrative care models. The National NCD Portal monitors millions of patients, facilitating data-driven policy and improving continuity of care. Innovative programs combine traditional Indian medicine with modern approaches, such as Ayurveda and Yoga, to enhance prevention and management holistically. Furthermore, telemedicine and digital health tools are extending diabetes care into rural and underserved regions, promoting equity. In my opinion, these multi-sectoral, technology-enabled interventions will be vital to controlling diabetes in the long term. Yet, ongoing evaluation and adaptation to India’s diverse needs remain imperative for success.
Special Programs on World Diabetes Day in India
On World Diabetes Day 2025, India witnessed a spectrum of special programs aimed at amplifying diabetes awareness and care across diverse communities. Chief among these was the “Madhumeha Vimarsha” initiative hosted by the Central Ayurveda Research Institute, Bengaluru, which focused on integrating Ayurveda, Yoga, and modern digital tools to enhance diabetes management and prevention. Alongside, free diabetes screening camps and workplace wellness workshops actively engaged citizens nationwide, underscoring the year’s theme, “Diabetes across life stages.” Incidentally, these programs reflect a valuable blend of traditional wisdom and contemporary science designed to reach India’s broad population effectively. Digital health platforms delivering teleconsultations and SMS alerts significantly expanded outreach to underserved regions, promoting early diagnosis and continuous care.
Additionally, public awareness campaigns included marathons, walkathons, and yoga sessions in urban and rural areas fostering community participation. Virtual seminars and educational treks aimed at empowering individuals through diabetes education further strengthened collective resilience. Importantly, coordinated efforts by government bodies, health institutions, and NGOs maximized program impact across states and socio-economic strata. As someone closely observing these campaigns, I believe that active community involvement combined with strategic government support is vital for sustained progress against diabetes. These initiatives not only increase awareness but also motivate lifestyle changes critical for reversing the disease’s trajectory in India.
Towards Holistic Changes – The Way Forward
India’s diabetes crisis demands urgent, holistic action combining prevention, treatment, and policy reform. Despite ongoing government initiatives like the “75 by 25” roadmap aiming to cover 75 million diabetics by 2025, only around 16% achieve adequate glucose control, revealing persistent gaps. From my perspective, addressing these shortcomings requires strong emphasis on lifestyle changes, affordable medicines, and expanded healthcare infrastructure. Furthermore, community empowerment through education and digital tools can shift diabetes care from reactive to proactive. Ultimately, reversing this epidemic depends on collective commitment from individuals, healthcare providers, and policymakers alike.
Looking ahead, innovative strategies including precision medicine, technology integration, and traditional therapies like Ayurveda will reshape diabetes management in India. Sustained investment, responsive policies, and evidence-based program evaluation are essential for success. From what I observe, the most effective approaches will blend accessible treatment with holistic support tailored to diverse populations. Now, more than ever, it is critical to act decisively – whether through lifestyle changes, advocacy, or supporting public health initiatives. Together, we can curb diabetes and improve millions of lives. The time to join this fight across life stages is now. Will you take that step today?
#WorldDiabetesDay #DiabetesAwareness #DiabetesInIndia #DiabetesCare #Healthylifestyle

Diabetes
All that you said are correct!
China is the number one followed by India.
The reasons are many:
• Heredity
• Lifestyle -sedentary
• Fast foods
• Low fibre diet
• Shunning home-made food etc.
When both parents work, they have no time to cook at home. So, they order food online
Online food has too much salt and additives and these are addictive.
The advent of the IT is the main culprit.
People now have lot of disposable income which they splurge on food rather than
outdoor activities.
Another important factor is Doctor-Pharma nexus.
Earlier they said the fasting sugar level is 100, now they say it could be up to 140.
So, all these years people with 100 mg sugar were unnecessarily popping up tablets to
control sugar.
Sometimes the so called ‘researchers’ come up with ideas like yellow of egg is
dangerous because it has cholesterol, Coconut oil is bad because it has cholesterol.
Ghee is bad because it has cholesterol. Now all these ideas have been reversed.
Cholesterol is an essential component of our brain; without it no myelin sheath around
the axons of neurons could be formed. It also helps in:
• Building new tissue and repairing existing tissue.
• Producing steroid hormones, including estrogen and testosterone.
• Creating bile in the liver, which is essential for digestion.
• Aiding in the production of vitamin D, which is crucial for bone health.
• Forming part of cell membranes, contributing to their structure and fluidity.
Demystification of computer by the Microsoft has opened a variety of search engines.
For every sundry reason people rush to Google and start self-medicating.
This puts enormous stress on our natural healing system which eventually affect our liver and pancreas.
So diabetes is not a simple problem; partly due to the Asian genome and partly because of our own folly.