
Numbers That Demand Our Attention
World Cancer Day 2026 arrives amid India’s largest health crisis nobody adequately discusses. Every 56 seconds in India, someone dies from cancer. That’s not merely a statistic – it represents interrupted lives, shattered families, economic catastrophes compressed into seconds. In spite, these numbers often remain abstract until they touch our own circles.
Our nation grapples with 2.5 million cancer patients currently living. Additionally, approximately 756,400 new cases emerge annually while 556,400 cancer deaths occur yearly.
What makes this World Cancer Day particularly significant is not new discovery but honest acknowledgment: prevention remains possible, screening saves lives, yet implementation gaps persist across regions, economic classes, and genders. This World Cancer Day invites examining why India’s cancer burden concentrates disproportionately among vulnerable populations despite available interventions.
The theme “United by Unique Journeys” acknowledges something essential: cancer experiences differ fundamentally based on geography, resources, gender, and caste. A farmer’s oral cancer journey differs entirely from an urban professional’s breast cancer experience. Yet, World Cancer Day asks us to witness all journeys with equal recognition of dignity and support.
Understanding World Cancer Day 2026 Theme in India’s Context
“United by Unique Journeys” – What This Actually Means for India
India’s cancer burden doesn’t distribute evenly across populations. Rather, it concentrates devastatingly among economically vulnerable communities. Importantly, geographic location determines screening access more powerfully than disease prevalence. Furthermore, gender-based inequities create entirely different prevention and treatment experiences.
The “United by Unique Journeys” framework specifically addresses these disparities. A cervical cancer diagnosis in urban Hyderabad triggers immediate specialist consultation, advanced imaging, and treatment options within weeks. Meanwhile, the same diagnosis in rural Bihar might involve months of diagnostic delays, limited treatment facilities, and impossible financial calculations. Incidentally, women have cervical cancer. However, their journeys remain utterly distinct.
World Cancer Day 2026 invites acknowledging that structural factors – not individual choices – primarily determine cancer outcomes in India. Poverty doesn’t cause cancer, yet poverty prevents access to treatment. Similarly, occupational hazards concentrate among unprotected workers while wealthy populations avoid carcinogenic exposures. Education levels influence screening awareness, yet rural populations often lack access regardless of awareness.
Integration of Traditional and Modern Medicine – A World Cancer Day Opportunity
India possesses ancient wisdom regarding holistic health that modern oncology increasingly validates. Ayurveda emphasizes balance across physical, psychological, and spiritual dimensions. Yoga and meditation demonstrate measurable anxiety reduction for cancer patients. These approaches complement rather than contradict modern chemotherapy and radiation.
Interestingly, research suggests integrated approaches improve treatment tolerance and psychological resilience. Dr. Arun Kumar Giri, Director of Surgical Oncology at Aakash Healthcare, emphasizes: “Modern cancer treatment focuses on tumor eradication, yet comprehensive healing must address the complete person – body, mind, and spirit. Integration of traditional wisdom with contemporary medicine produces superior outcomes.” This perspective reframes World Cancer Day not as biomedical intervention alone but as holistic restoration.
Current practice rarely implements this integration. Most Indian cancer centers focus exclusively on chemotherapy, radiation, and surgery. Mental health services remain virtually non-existent outside metropolitan hospitals. Consequently, patients either access traditional practitioners separately or forgo complementary support entirely. What World Cancer Day 2026 might validate: genuine healing requires multiple knowledge systems working together.
Cancer Statistics in India: Understanding the Burden Through Data
A Decade of Escalation – What Trends Reveal About Prevention Failure
Cancer incidence in India has escalated persistently over ten years. In 2016, approximately 700,000 new cases emerged annually. Subsequently, by 2020, this figure reached 735,000 cases. Moreover, current 2026 projections indicate approximately 800,000 new cases – a 43.5% increase over one decade. Concurrently, annual cancer deaths increased from 475,000 to 556,400, representing a 17.2% mortality increase.
This escalation is largely preventable. Tobacco consumption drives approximately 40% of India’s cancer burden. Additionally, lifestyle factors (obesity, physical inactivity, dietary patterns) contribute to rising incidence. Furthermore, occupational exposures remain inadequately regulated despite known carcinogenic hazards. Notably, these trends suggest that World Cancer Day prevention strategies have reached only narrow segments of the population.
The age distribution deserves particular attention. Approximately 71% of cancer deaths occur between ages 30-69 – India’s most economically productive decades. Consequently, cancer disrupts family financial stability, educational opportunities for children, and long-term economic planning. A single cancer diagnosis can unravel decades of accumulated savings and create multigenerational poverty.
Gender-Specific Epidemiology – Why Male and Female Cancers Demand Different Interventions
Male and female cancer patterns diverge dramatically in India. Among men, oral and lip cancers dominate at 13.51% of total male cancer cases (approximately 102,200 cases annually). Subsequently, lung cancer represents 9.65%, stomach cancer comprises 8.2%, while pharyngeal cancers constitute 7.5%. Notably, these cancers correlate strongly with tobacco and alcohol consumption patterns concentrating among occupational groups.
Female cancer patterns differ substantially. Breast cancer leads at 28.2% of female cases (125,000 cases annually). Subsequently, cervical cancer represents 22.86% (101,000 cases annually). Importantly, both represent largely preventable diseases through screening and vaccination. However, prevention infrastructure concentrates in metropolitan areas, creating vast rural-urban screening gaps. Consequently, women in underserved regions experience late-stage diagnoses and worse outcomes despite similar disease biology.
Dr. Ashok Kumar Vaid, a leading hemato-oncologist at Medanta Hospital, observes: “Gender-specific cancer patterns in India reflect not biological differences but access disparities. Cervical cancer remains preventable through HPV vaccination at 95% effectiveness, yet rural coverage remains below 30%. This represents systemic failure, not individual shortcoming.” This insight reframes World Cancer Day prevention messaging from individual responsibility toward structural accountability.
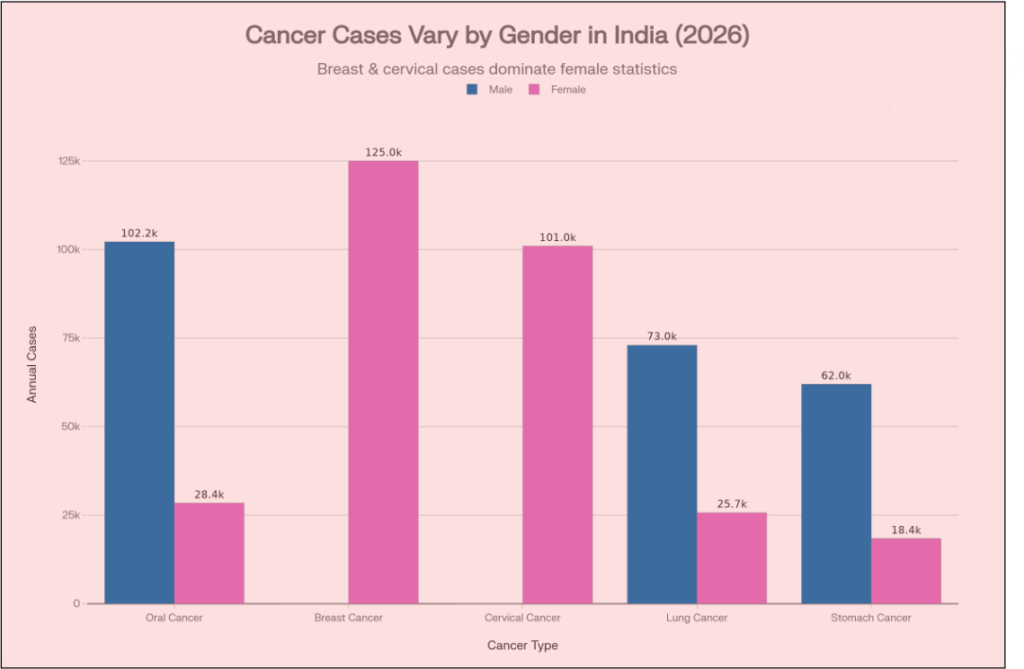
Source: National Cancer Registry Programme (NCRP), India – 2025-2026 official data
Gender-Specific Cancer Patterns and Prevention Status in India
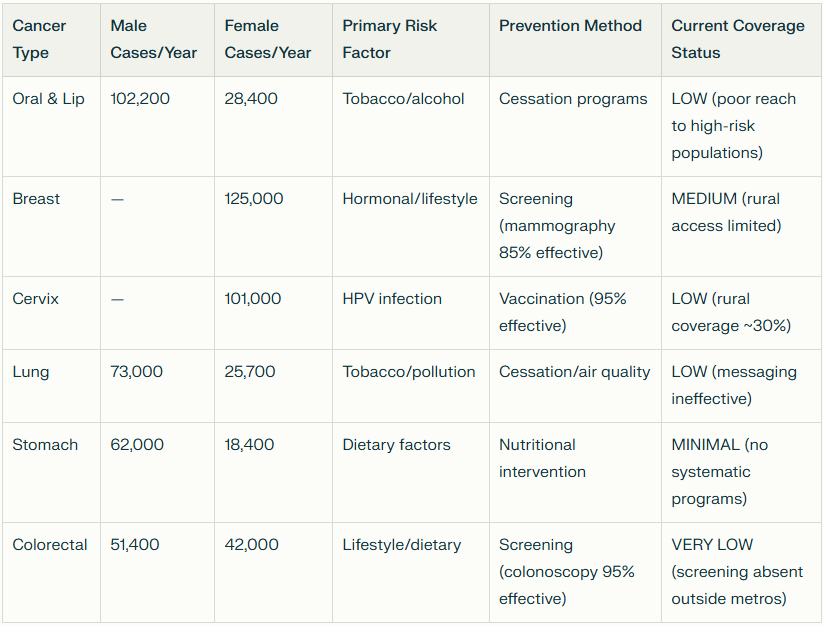
Source: National Cancer Registry Programme (NCRP), 2026
Key Insight: Cancers most preventable through vaccination or screening show lowest implementation coverage, particularly in rural India.
Major Risk Factors : Where World Cancer Day Strategy Falters
Tobacco – The Preventable Crisis India Inadequately Addresses
Tobacco represents India’s most consequential modifiable cancer risk factor. Directly, it causes approximately 2,500 deaths daily through oral, lung, and pharyngeal malignancies. Among Indian men, tobacco accounts for 1 in 5 deaths annually. Additionally, among women, tobacco causes 1 in 20 deaths – not because women face lower risk but because smoking prevalence remains lower while chewing tobacco remains understudied.
What complicates tobacco prevention is how it concentrates among economically vulnerable populations. A construction worker earning ₹400 daily might spend ₹50 on tobacco – that’s 12.5% of income directed toward addiction. Still, corporate marketing deliberately targets lower-income communities through affordable products and unregulated advertising. Consequently, tobacco prevention requires structural intervention, not merely individual willpower.
Interestingly, India could prevent approximately 400,000 cancer cases annually through comprehensive tobacco control. However, implementation remains inconsistent. The Cigarette and Other Tobacco Products Act (COTPA) theoretically restricts advertising and regulates public consumption. However, enforcement varies dramatically across states. Rural areas experience minimal regulation while informal markets continue peddling uncontrolled products. Thereby, World Cancer Day prevention messaging must shift from individual exhortation toward demanding corporate accountability and occupational health protections.
Screening Infrastructure – Why Prevention Remains Geographically Unequal
Early cancer detection transforms outcomes fundamentally. A screened breast cancer caught at stage 1 achieves 92% five-year survival. Meanwhile, advanced-stage breast cancer reaches only 72% survival – a 20-percentage-point difference determining life versus death. Similarly, cervical cancer screening achieves 90% effectiveness, yet current coverage reaches merely 10-15% of eligible populations.
The National Cancer Screening Programme theoretically mandates cervical, breast, and oral cancer screening. However, actual implementation resembles fragmented patchwork. Metropolitan areas conduct regular screening camps with adequate equipment and trained personnel. Rural districts report sporadic programs, often suspended without notice. Consequently, geography rather than disease biology determines screening access. A woman in Delhi accesses regular mammograms while her cousin in rural Odisha may never receive one.
This infrastructure gap persists despite known solutions. Mobile screening units could reach underserved communities. Integration with primary healthcare could expand reach. Community health workers could conduct initial screening with specialist consultation via telemedicine. However, these require systematic investment, coordination, and funding commitments which are currently absent. Importantly, this World Cancer Day 2026 must acknowledge that screening gaps represent policy failure, not individual oversight.
Distribution of Major Cancer Types Across India
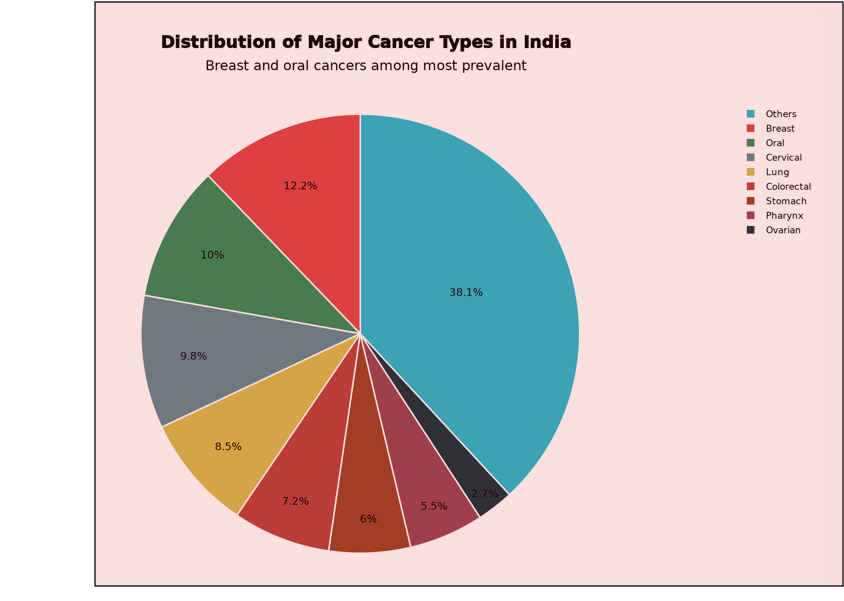
Source: National Cancer Registry Programme (NCRP)
Healthcare Access and Financial Toxicity: Structural Barriers to Treatment
The Economics of Cancer – Why Financial Barriers Eclipse Medical Barriers
Cancer diagnosis precipitates simultaneous medical and financial crises. Average treatment costs range from ₹5-15 lakh, representing 2-10 times annual income for median Indian households. Consequently, most families cannot afford treatment without asset liquidation, borrowing, or treatment discontinuation. This creates impossible choices: continue chemotherapy or preserve family savings? Pursue surgery or maintain house payments?
Government schemes like Ayushman Bharat theoretically address this through insurance covering cancer treatment up to ₹5 lakh. Despite this, coverage remains inadequate for many cancers requiring extended treatment or advanced therapeutics. Furthermore, implementation inconsistencies prevent many eligible beneficiaries from accessing promised support. Moreover, documentation requirements confuse beneficiaries unfamiliar with bureaucratic processes. Besides, authorization delays postpone treatment beyond medically optimal timing. Thereby, insurance schemes remain largely theoretical rather than practically accessible.
Importantly, financial stress actively harms cancer outcomes. Patients discontinue treatment prematurely due to cost exhaustion. They skip nutritional support, follow-up appointments, and psychological counseling. Consequently, financial toxicity creates secondary health crises layered atop disease burden. A patient carries simultaneous burdens: cancer attempting to kill them, and financial systems pushing them toward bankruptcy. This dual burden demands structural reform beyond current government schemes.
Rural-Urban Divide – Geography as Destiny for Cancer Outcomes
India’s cancer mortality concentrates geographically with stark rural-urban disparities. Urban centers like Hyderabad, Delhi, and Chennai possess advanced oncology infrastructure, specialist availability, and treatment options. Meanwhile, rural districts lack basic diagnostic facilities, forcing patients into costly metropolitan travel. Consequently, geography determines cancer survival more powerfully than the disease itself.
Rural patients navigate particular hardships. Suppose a farmer receives cancer diagnosis in rural Maharashtra. He must travel 150+ kilometers to a city hospital for specialist consultation. In addition, treatment typically requires repeated metropolitan visits over months – perhaps 30-50 trips. Transportation, accommodation for family members, and lost agricultural income multiply treatment costs substantially. Indirectly, these costs often exceed direct medical expenses.
This rural disadvantage concentrates among vulnerable populations least able to absorb costs. A construction worker, agricultural laborer, or informal sector employee lacks employer health insurance, paid medical leave, or savings cushion. Consequently, cancer diagnosis triggers simultaneous crises: disease, lost income, displaced employment, family separation. What World Cancer Day 2026 must acknowledge: these aren’t individual misfortunes but systemic failures requiring infrastructure investment in underserved regions.
Survival Rate Disparities – What India’s Gaps Actually Represent
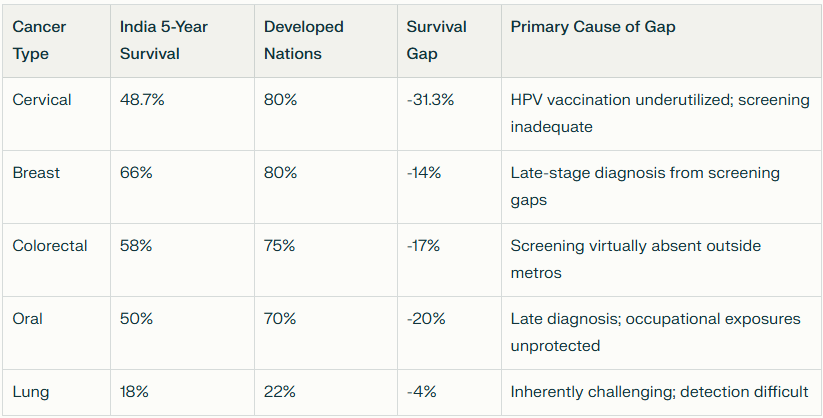
Source: National Cancer Registry Programme (NCRP), 2025
Critical Interpretation: The cervical cancer gap (-31.3%) between India and developed nations doesn’t reflect biological differences. Rather, it represents India’s failure to implement HPV vaccination (95% effective) and cervical screening (90% effective) systematically. This gap represents preventable deaths – a policy choice, not medical inevitability.
Screening and Early Detection: The Democracy That Remains Inaccessible
The Privilege of Early Detection – Why Screening Access Determines Survival
Early detection fundamentally transforms cancer outcomes. This fact remains indisputable across all cancer types. A screened cancer caught early achieves survival rates 40-50 percentage points higher than advanced presentations. Sadly, screening access concentrates so thoroughly in metropolitan areas that early detection effectively becomes a privilege of affluent urban populations.
Currently, cancer screening reaches perhaps 10-15% of eligible populations. Metropolitan areas conduct regular screening camps with adequate equipment, trained personnel, and follow-up protocols. Rural districts remain largely unscreened. Consequently, cancers progress undetected while screening infrastructure sits underutilized in metropolitan centers. This represents not just inequity but profound resource misallocation.
Particularly troubling is cervical cancer screening. HPV-based testing or Pap smears remain highly effective (90%+ effectiveness). However, such screening facilities remain concentrated in urban clinics where educated, affluent women access regular screening. On the other hand, rural women – at highest cervical cancer risk due to limited preventive care – experience sporadic or non-existent screening programs. Therefore, it has to accepted that prevention infrastructure fails populations most needing it.
Mental Health Integration – The Neglected Dimension of Cancer Care
Cancer’s psychological burden frequently rivals or exceeds its physical toll. Diagnosis precipitates crisis: patients confront mortality, anticipated suffering, potential disability, and financial devastation simultaneously. Additionally, post-treatment phases introduce distinct psychological challenges: existential questions about life’s meaning, anxiety about recurrence, and complicated grief over altered identity.
Surprisingly, psycho-oncology services remain virtually non-existent outside major metropolitan cancer centers. Most Indian patients navigate cancer journeys without specialized psychological support. Some receive unhelpful messaging – “stay positive” (implying negativity caused cancer), “think of your family” (adding responsibility to burdened patients), “others have it worse” (invalidating legitimate suffering).
What would genuine mental health integration look like? Psycho-oncology specialists trained specifically in cancer-related trauma. In addition, support groups facilitating honest conversation rather than inspirational narratives. Also, therapy addressing existential questions accompanying diagnosis. Pitifully, these remain visibly absent to a large extent. Importantly, World Cancer Day 2026 might validate that psychological support ranks equivalent to chemotherapy in importance. Comprehensive cancer care requires addressing whole persons, not merely tumors.
Government Initiatives 2026: Progress, Promises, and Persistent Gaps
“Towards a Cancer-Free India” – Commitments on Paper Versus Implementation
The Indian government articulated ambitious objectives under “Towards a Cancer-Free India” framework launched February 2025. This emphasizes prevention, early detection, affordable treatment access, and rehabilitation support. Theoretically, it guides systematic policy. In practice, observers witness persistent gaps between promise and implementation.
A landmark commitment involves establishing 200 Day Cancer Care Centers by 2026. These outpatient facilities would provide chemotherapy, supportive care, and follow-up visits within communities. On paper, this eliminates costly hospitalization. Practically, critical questions emerge: Will facilities maintain adequate staffing? Will they stock necessary medications consistently? Will they uphold quality standards? Will rural communities actually access them given transport barriers? These details determine whether policy translates into lives saved.
The National Cancer Registry Programme expanded its network. Currently, 43 cancer registries operate across India collecting epidemiological data. This theoretically enables evidence-based resource allocation and policy formulation. However, data collection remains inconsistent across regions. Rural areas register substantially fewer cases than metropolitan areas – suggesting underreporting rather than lower actual burden. Better data matters only if it is transformed into systematic action.
Ayushman Bharat and Insurance Coverage – Why Schemes Remain Inadequate
Ayushman Bharat scheme expanded nominally covering 500 million individuals through ₹5 lakh cancer treatment insurance limits. Still, coverage remains inadequate relative to actual treatment costs. Many cancers exceed ₹5 lakh considerably, leaving patients responsible for substantial out-of-pocket expenses. Furthermore, implementation inconsistencies abound.
Some patients discover coverage exists only at specific network hospitals located far from their homes. Others encounter authorization delays that postpone treatment beyond medically optimal timing. Documentation requirements confuse beneficiaries unfamiliar with bureaucratic processes. Thereby, insurance schemes represent theoretical rather than practical solutions for vulnerable populations needing support most.
What’s absent from government initiatives is coordinated systemic intervention. Rural infrastructure remains underfunded. Mental health integration remains virtually non-existent. Tobacco industry regulation remains inconsistent. Prevention messaging reaches educated urban populations while bypassing vulnerable communities most needing intervention. World Cancer Day 2026 must acknowledge these pressing issues: current government commitments represent beginning steps, and non-comprehensive solutions to India’s cancer crisis.
Holistic and Integrated Care: Validating Traditional Knowledge Systems
Evidence for Traditional Approaches – What Research Demonstrates
India possesses extraordinary advantages in holistic cancer care given rich philosophical traditions emphasizing integrated health. Yoga and meditation demonstrate measurable anxiety reduction for cancer patients. Research suggests improved sleep quality, enhanced treatment tolerance, and reduced side effects. Strangely, yoga remains conspicuously absent from most cancer treatment protocols despite evidence supporting effectiveness.
Ayurvedic nutrition approaches support treatment tolerance and recovery. Meditation addresses existential dimensions of cancer diagnosis that chemotherapy cannot touch. These approaches complement rather than contradict modern medicine when thoughtfully integrated. Importantly, they resonate culturally with Indian patients in ways Western biomedical frameworks often don’t.
Some leading oncology centers have begun integration. Results suggest improved patient satisfaction, better treatment adherence, and enhanced psychological resilience. Notably, these remain exceptional institutions rather than standard practice across Indian cancer care. Most programs remain biomedically focused, dismissing traditional approaches as unscientific despite emerging evidence supporting effectiveness and patient preference.
Integration Models – Moving Beyond Biomedical Reductionism
What would genuine holistic integration look like? A cancer patient receives chemotherapy on Monday, attends yoga on Tuesday, consults an Ayurvedic practitioner on Friday – all within an integrated framework addressing whole persons. Currently, patients accessing traditional practitioners do so separately, often discontinued from medical treatment in false dichotomy.
Dr. Rupak Giri, an accomplished oncologist-researcher, notes: “Comprehensive cancer care must transcend biomedical reductionism toward integrated approaches honoring physical, psychological, and spiritual dimensions. Traditional Indian systems offer validated tools addressing dimensions modern medicine cannot, not as alternatives but as complementary components.” This perspective reframes World Cancer Day messaging toward genuine integration rather than dismissive tolerance of traditional approaches.
Implementing such integration requires infrastructure investment, practitioner training, and institutional policy changes. Besides, the benefits justify the effort: improved patient experience, potentially enhanced outcomes, and culturally appropriate care resonating with patients’ worldviews. World Cancer Day 2026 might validate that comprehensive healing requires multiple knowledge systems – modern medicine excelling at tumor treatment along with traditional approaches excelling at supporting persons navigating the disease.
Community and Grassroots Action: When Systems Fail, Communities Act
Survivor Networks and Peer Support – Healing Through Shared Experience
Beyond government and hospitals, remarkable community movements have emerged to address gaps in formal systems. Survivor networks operate across major Indian cities where cancer survivors support current patients through peer understanding that healthcare providers cannot replicate. They provide practical advice about managing treatment side effects, navigating financial barriers, and communicating with families about their experiences.
These networks demonstrate something essential: shared experience creates credibility and connection beyond clinical expertise. A survivor explaining chemotherapy fatigue reaches a patient differently than medical literature. A caregiver describing emotional burden validates experiences that patients fear naming aloud. Thereby, survivor networks address psychological and practical gaps that formal systems leave open.
Organizations like CanSupport and Indian Cancer Society operate support hotlines, facilitate support groups, provide financial assistance to vulnerable patients, and connect patients with community resources. These services address gaps that government systems fail to provide. Importantly, grassroots efforts demonstrate that when communities recognize cancer as a shared challenge, they mobilize resources and determination exceeding what formal systems can generate.
Occupational Health and Women’s Health Advocacy – Structural Intervention
Occupational health advocates document oral cancer burden among construction workers, agricultural laborers, and tobacco workers. Additionally, they mobilize unions and workers’ organizations to demand occupational health protections and tobacco cessation support as worker rights. Thereby, they reframe cancer prevention from individual behavior change toward structural intervention addressing exploitative labour conditions enabling tobacco use.
Women’s organizations have launched cervical cancer awareness campaigns navigating cultural sensitivities in conservative communities. They advocate for HPV vaccination and screening despite religious and patriarchal objections. These efforts demonstrate that bottom-up movements can effectively address structural barriers preventing access.
Workplace wellness programs, particularly within corporate organizations, increasingly incorporate cancer screening camps and awareness sessions. Importantly, occupational settings provide accessible touchpoints for reaching working-age populations at peak cancer risk. These initiatives demonstrate screening integration feasibility within existing community structures.
What Readers Can Do: Individual Actions Within Systemic Framework
Personal Prevention and Health-Seeking Behaviour – Practical Steps
World Cancer Day invites practical personal engagement while acknowledging that individual action alone cannot resolve systemic failures. For those able to access healthcare, regular cancer screening when eligible becomes fundamental. Women should pursue cervical cancer screening through HPV testing or Pap smears. Importantly, recognizing breast cancer early warning signs through self-awareness complements clinical screening.
Tobacco cessation remains the single most impactful personal intervention. Additionally, abstinence or moderate alcohol consumption, regular physical activity, healthy nutrition, and stress management through yoga or meditation substantially reduce cancer risk. These modifications simultaneously improve overall health and wellbeing across multiple dimensions. Importantly, these actions remain accessible to individuals regardless of socioeconomic status.
Supporting cancer patients within personal and professional networks matters substantially. Showing up, listening without attempting to fix, and accepting legitimate fear and grief without demanding positivity – these simple acts provide crucial support. Additionally, advocating for colleagues’ and family members’ screening participation despite potential discomfort represents practical engagement.
Collective Action and Systemic Advocacy – Moving Beyond Individual Prevention
The danger with cancer prevention messaging is individualizing the disease, suggesting cancer results from personal choices rather than acknowledging structural forces shaping health. A construction worker breathing silica dust daily cannot exercise away occupational lung cancer risk. A farmer exposed to pesticides cannot diet his way to health. A woman without transport cannot willpower her way to screening access.
World Cancer Day 2026 poses to you some pertinent questions: what are you willing to advocate for within your sphere of influence? Regulating corporate marketing that targets vulnerable populations? Demanding occupational health standards that protects vulnerable workers? Ensuring screening infrastructure in underserved regions? Supporting financial security enabling people to prioritize health? These require collective action, policy change, and resource allocation.
Importantly, systemic change emerges from sustained engagement, not grand gestures. Supporting NGOs providing patient support, advocating for policy change toward equitable care systems, engaging in electoral processes demanding candidate commitment to cancer control – these represent genuine collective action. World Cancer Day ultimately invites recognizing cancer control as a shared responsibility transcending individual prevention toward systemic transformation.
What World Cancer Day 2026 Invites Us to Acknowledge
World Cancer Day exists to transform statistics back into human stories while simultaneously demanding structural examination of why some people can access cancer care while others die from this preventable disease. This year’s theme, “United by Unique Journeys,” acknowledges that cancer experiences differ fundamentally based on geography, resources, gender, and caste.
Understanding India’s cancer crisis requires confronting uncomfortable truths: prevention remains possible, yet implementation reaches narrow population segments. Screening saves lives, yet infrastructure concentrates in metropolitan areas. Treatment exists, yet financial barriers prevent access for millions. Mental health support matters, yet remains virtually non-existent. Systemic change appears necessary, yet political will remains inadequate.
On a positive note, grassroots movements, government initiatives, individual engagement, and growing awareness suggest that transformation remains possible. On World Cancer Day 2026, the invitation extends beyond statistics toward genuine reckoning: examining what our systems serve and whom they fail, acknowledging structural barriers while mobilizing personal and collective action, validating multiple knowledge systems while demanding evidence-based policy, and ultimately recognizing cancer control as shared responsibility transcending individual responsibility.
The statistics remain stark: 1,525 daily deaths, 756,400 annual cases, 2.5 million currently living with cancer. Behind each number stands a unique journey deserving dignity, comprehensive care, and systemic support. This World Cancer Day, that recognition might become the beginning of genuine change.
At ExpressIndia.info, we are collaborating with various NGOs to amplify cancer awareness and connect readers with accessible support services across India. We encourage our readers to recognize cancer as a collective responsibility, prioritize preventive health measures, and demand systemic change that ensures no individual’s cancer journey unfolds in isolation or despair🎗️💪🏥🤝💚. Express yourself and let your voice be heard aloud. 🗣️🎤📢💕
#WorldCancerDay2026 #CancerAwarenessIndia #UnitedByUniqueJourneys #CancerPreventionMatters #HealthEquityIndia
